Combining Guided Intervention of Education and Relaxation (GIER) with Remote Electrical Neuromodulation (REN) in the Acute Treatment of Migraine
Dawn C. Buse et al, Pain Medicine, 2022
Abstract
Background
Evidence indicates that combining behavioral treatments with pharmacological treatments for migraine prevention improves efficacy, however little is known about the outcomes of combining neuromodulation and behavioral interventions for acute treatment of migraine. Remote Electrical Neuromodulation (REN) is an FDA-cleared non-pharmacological migraine treatment. The current study evaluated the clinical benefits of augmenting REN treatment with a specially tailored behavioral therapy comprised of Guided Intervention of Education and Relaxation (GIER), for the acute treatment of migraine.
Methods
In this two-arm observational study, real-world data were collected from patients across the United States who were using the REN device. Eighty-five migraine patients aged ≥18, who treated their attacks with REN in parallel with the GIER intervention were individually matched on age and sex with 85 patients who used REN alone. The groups were compared on the proportion of migraine attacks in which they achieved pain relief, pain freedom, improvement of function, and return to normal function, at 2 hours post-treatment.
Findings
Data from 170 users were analyzed (85 per group). Compared to the REN-only group, the REN+GIER group displayed statistically significant higher proportion of patients achieving consistent pain relief (p=0.008), consistent improvement in function (p=0.014), and consistent return to normal function (p=0.005); all at 2 hours post treatment.
Conclusions
The results suggest that combining the GIER behavioral intervention with REN treatment can improve the therapeutic efficacy beyond that of REN alone, in terms of both pain level and improvement of disability.
Keywords: Nerivio, remote electrical neuromodulation, migraine, headache, behavioral, digital therapeutics.
Introduction
Data supported, guideline recommended biobehavioral therapies with proven efficacy for migraine prevention include biofeedback, cognitive behavioral therapy and relaxation training (1–4). These treatments can reduce migraine attack frequency, associated disability, psychological symptomology and improve related quality of life (5–7). Furthermore, the integration of behavioral therapies with pharmacological preventive treatment has been shown to be more effective compared to either therapy alone (8). Relatedly, incorporating psycho-education about the biology of pain and the brain’s ability to modulate pain is a mainstay of comprehensive migraine management and has been shown to improve the efficacy of acute treatment (9,10).
Remote electrical neuromodulation (REN) is a non-pharmacological, non-invasive, neuromodulatory treatment that stimulates nociceptive nerve fibers in the upper arm to activate an endogenous descending pain inhibition mechanism termed Conditioned Pain Modulation (CPM) (11–13). REN has been shown to be safe and effective for the acute treatment of migraine in adults with episodic (14–16) and chronic migraine (17,18), and in adolescents with migraine (19).
The Guided Intervention of Education and Relaxation (GIER) is a relaxation and education guided audio and visual intervention designed for use with REN treatments. It is a 25-minute video, played on the user’s smartphone during REN treatment, comprised of training in three relaxation techniques: diaphragmatic breathing, progressive muscle relaxation, and guided imagery, as well as pain education content on migraine biology and REN treatments.
The current study evaluated the clinical benefits of augmenting REN with the GIER behavioral intervention for the acute treatment of migraine, in an observational, real-world setting.
Materials and methods
Design and setting
This was a retrospective observational matched case-control investigation, in which data from patients with migraine who chose to integrate GIER into their REN treatment were individually matched with data from patients who used REN alone.
All participants had the Nerivio (™) app installed on their smartphones, and accepted the terms- of-use which specify that providing personal information is done of their own free will, and that their de-identified data may be used for research purposes. Users were not obligated to provide personal information (i.e., they may treat without providing feedback). The app includes a migraine diary, which enables patients to track pain and disability.
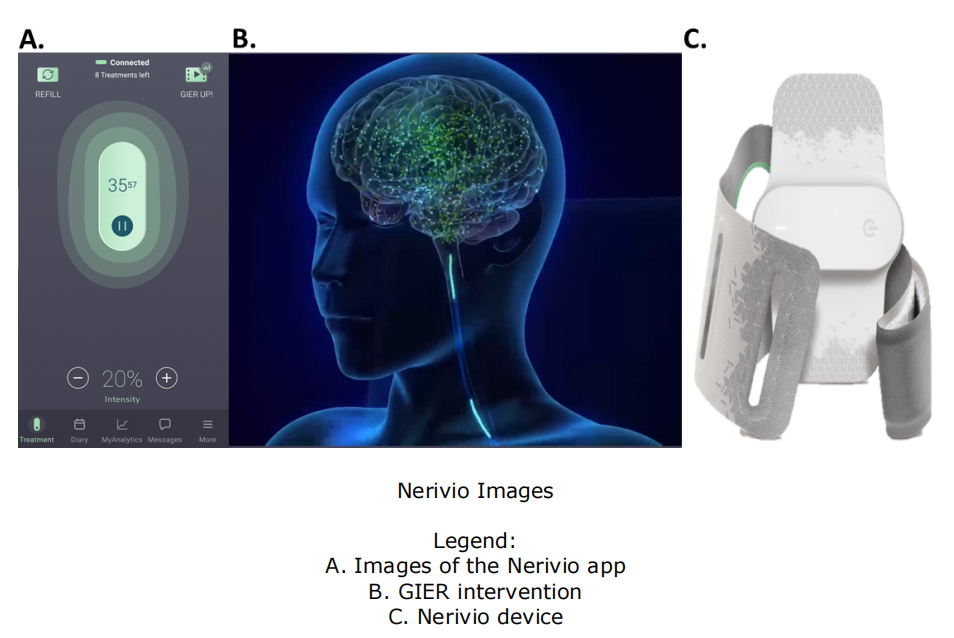
A GIER icon was made available on the Nerivio app for all REN users following a software-update (‘GIER UP’ icon, figure 2), and no additional information whatsoever was provided on GIER prior to viewing the video to prevent expectation bias.
Participants
The data were collected from patients across the United States who used REN with or without GIER between March 8, 2020 and April 19, 2021. Patients provided consent for the use of their anonymized data for research purposes during sign-up for the Nerivio app.
The inclusion criteria for the combined intervention group (REN+GIER) consisted of all patients with two or more REN+GIER treatments in which pain ratings were available at pre-treatment and 2 hours post-treatment, and no rescue medications were taken within 2 hours from treatment onset. All subjects had a minimum of 30 minutes per REN treatment, and the minimum for GIER duration was 7 minutes. No selection was done on this sample, and all qualifying subjects were included.
The control group (REN only) consisted of GIER-naïve patients, with otherwise same inclusion criteria.
For each person in the REN+GIER group, we randomly sampled a user from the control group matched on sex and age (±2 years, priority given to exact matches). Matching was done blindly in terms of efficacy results, so that subjects were first matched (with no replacement) and only then their efficacy data were retrieved.
REN device
The REN device and its mechanism of action have been described in detail elsewhere(14,20). Briefly, it is an FDA-cleared prescription device, controlled by a phone application. It is worn on the upper arm at the onset of migraine headache, and stimulates C and Aδ nociceptive fibers for 45 minutes, to activate the CPM.
GIER intervention
The GIER intervention is a 25-minute video that can be played on the user’s smartphone. The video becomes available upon starting the REN treatment, by clicking a small icon in the top right corner of the app’s screen. The video provides educational information about migraine, and practice in three relaxation techniques: progressive muscle relaxation, diaphragmatic breathing, and guided imagery. For progressive muscle relaxation, patients receive instructions to stretch and relax certain muscle groups focusing on the head, face, jaw, neck, and shoulders. Diaphragmatic breathing training provides instructions for paced breathing, engaging the stomach and abdominal muscles. Guided imagery offers suggestions for the disappearance of pain. The pain education content focuses on migraine biology emphasizing that migraine pain is not dangerous, and education on how REN treatments work. At any point during the video, the user can choose to switch to audio only, or to stop the video (and the REN treatment will continue to go on as usual). The operation of the GIER feature is done separately for each treatment session, so that augmenting the REN treatment with GIER in one treatment session, has no bearing on the following treatments. Figure 2 presents an image of the app’s screen during treatment, an image from the GIER video, and a picture of the Nerivio device.
To reduce a potential placebo effect, patients received no information about the potential benefit of this intervention, nor specific instructions for its use.
Results
Outcome measures
Outcome measures were collected using an electronic diary embedded within the Nerivio app. Users were prompted to fill the diary before the REN treatment and at 2 hours post treatment.
Pain intensity was rated on a 4-point scale (none, mild, moderate, or severe). Functional disability also was rated on a 4-point scale (no limitation, some limitation, moderate limitation, severe limitation). Pre-post changes in these measures were used to derive the following primary outcome variables: ‘Pain relief’ was defined as a pre-post change from moderate or severe pain intensity to mild or none; ‘pain freedom’ was defined as a report of no pain on the 2-hour post- treatment diary; functional improvement’ was defined as a pre-post improvement by at least one level; and ‘return to normal function’ was defined as a report of no limitation on the 2-hour post- treatment diary. Consistency was defined as at least 50% of treatments in which response (pain relief/ pain freedom/ functional improvement/ return to normal function) was achieved, per person.
Outcome measures indices were coded as a response/no response, per treatment.
Data analysis
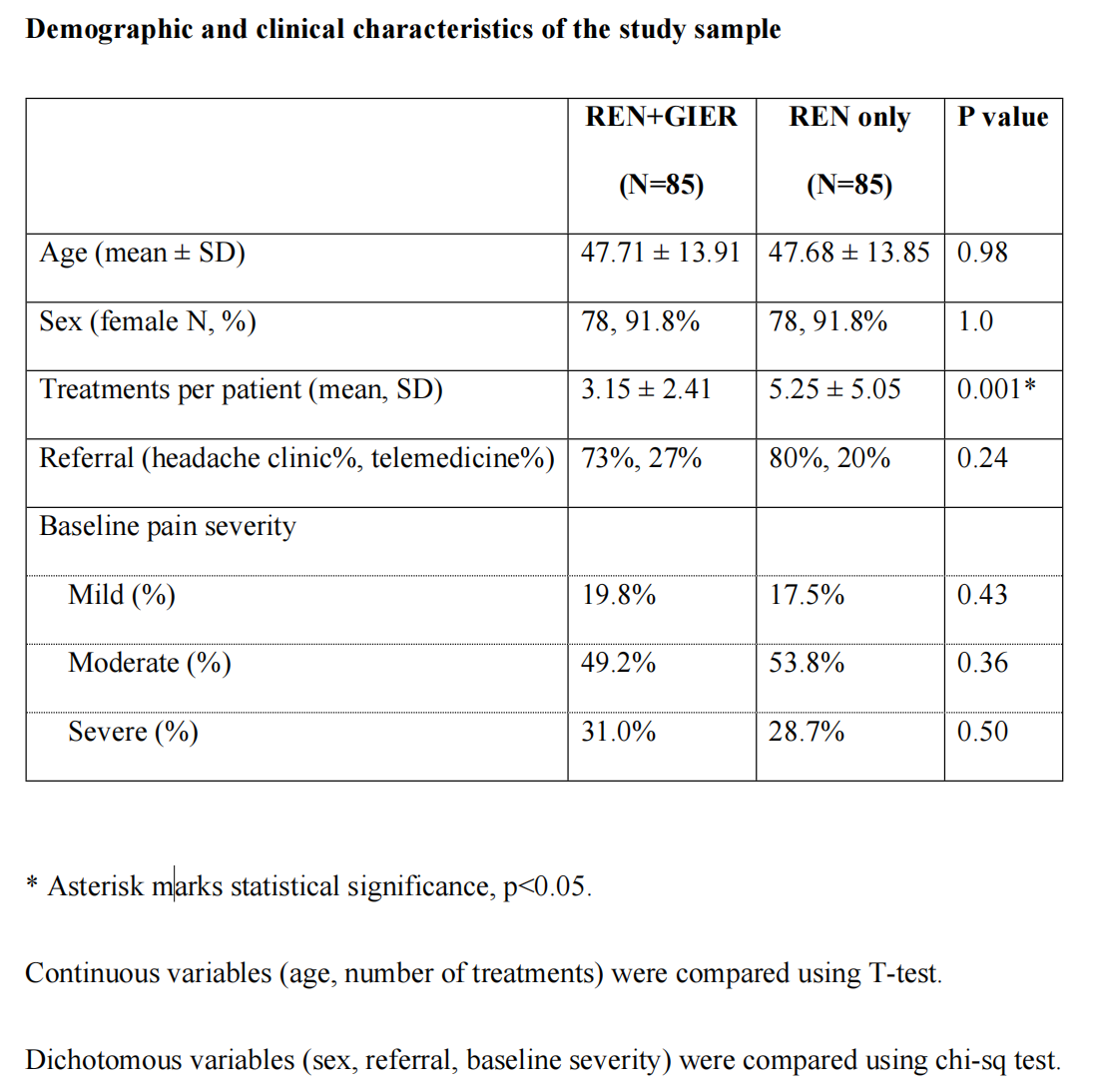
The percentage of patients in each group that achieved response in each parameter was calculated. Group differences were evaluated using the chi-squared test for dichotomous variables (response/no response, sex, baseline severity), and T-tests for continuous variables (age, number of treatments). All tests were two-tailed, with a p=0.05 threshold. All data used for the analyzes presented herein is available upon request from the authors. This is the primary analysis of these newly collected data.
There were no missing data, by design (see inclusion criteria).
Results
Data from 170 users was analyzed (85 per group), 92% of participants were women, participant’s mean age was 47.7±13.9; clinical and demographic data are presented in Table 1. Most participants (76.5%) were referred to use the REN device by headache specialists. Of the analyzed sample, 51.5% of the patients experienced moderate headache levels at baseline and 30% experienced severe headache. There were no differences between the groups in baseline characteristics in terms of age, sex, baseline pain severity, or source of referral. The average number of treatments per patient was higher in the REN-only group (see table 1).
Response to treatment results are presented in Figure 1.
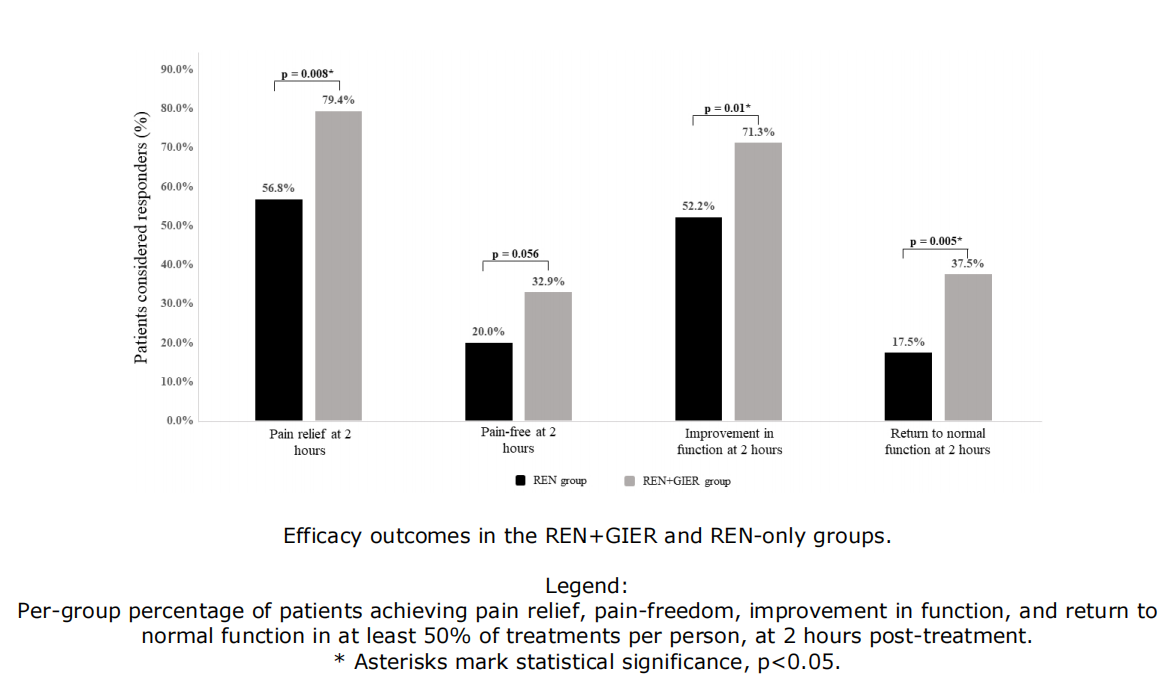
Compared to the REN-only group, the REN+GIER group had statistically significant higher proportions of patients achieving:
Consistent pain relief (REN+GIER responders N=50, 79.4%; REN-only responders N=42, 173 56.8%; p=0.008).
Consistent improvement in function (REN+GIER responders N=57, 71.3%; REN-only responders N=42, 52.5%; p=0.014).
Consistent return to normal function (REN+GIER responders N=30, 37.5%; REN-only responders N=14, 17.5%; p=0.005).
Consistency of pain freedom was qualitatively higher in the REN+GIER group, but the difference did not reach statistical significance (REN+GIER responders N=28, 32.9%; REN-only responders N=17, 20.0%; p=0.056).
Discussion
This real-world evidence study indicates that augmenting REN with the new GIER behavioral intervention can improve the therapeutic efficacy beyond that of REN alone, in terms of the percentage of participants achieving consistency of pain relief, consistency of improvement in function, and consistency of return to normal function (the ratio of consistent pain freedom was qualitatively higher in the GIER group, but did not reach statistical significance).
The GIER intervention combines three relaxation approaches (progressive muscle relaxation, diaphragmic breathing, and guided imagery) and an educational component. Combining behavioral approaches has been shown to be more effective for headaches than each method alone (22), especially for acute pain (23). Availability of several behavioral-treatment options also allows patients with different preferences an opportunity to integrate behavioral strategies into treatments (24,25). Additionally, the use of a smartphone app has the potential to increase adherence with the intervention, as people with migraine report preference to smartphone-based behavioral therapies due to access barriers to traditional clinic-based delivery (26). Use of an app for delivery increases accessibility and is cost-effective, which are main barriers to the initiation of behavioral interventions (27,28). In addition, the use of behavioral approaches for acute treatment, i.e., treating when the attack has started, may overcome the adherence challenges posed by the longer commitment to training that is typically required in traditional, clinic-based, in-person behavioral interventions(29,30).
It should be noted that the REN-only group has a higher average number of treatments per person than the GIER group, however, this is expected since REN treatments can be performed together with daily activities, while the behavioral intervention requires time and attention dedicated to watching the video and engaging with the exercises. Given that outcome measures were calculated across the performed treatments per person,this has no bearing on the results.
This study’s main limitation is its observational nature. Future prospective random-allocation studies are needed to further establish the current results and to explore longer-term use. However, the observational real-world design has the advantage of providing valuable information on real-life effectiveness of the studied interventions.
Conclusion
this real-world evidence study suggests that combing the new GIER behavioral intervention with REN treatment can improve the therapeutic efficacy beyond that of REN alone, in terms of both pain level and improvement of disability.
List of abbreviations
1. GIER - Guided Intervention of Education and Relaxation
2. REN - Remote Electrical Neuromodulation
3. CPM - Conditioned Pain Modulation
